Medical Negligence Claims: Improper Fetal Monitoring in Labour and Birth
Fetal heart rate monitoring is a lifesaving skill as it enables health care providers to monitor the wellbeing of a fetus during labour and birth. When a neonate suffers injury because of labour or birth, regular fetal monitoring can be used to tell a narrative to explain how and when the baby deteriorated.
Improper fetal monitoring can occur through either.
- A failure to monitor when indicated.
- Improper or incorrect interpretation of fetal monitor traces
- Misreading or confusing the heart rates of the mother and baby
- Failure to take appropriate action when fetal distress is indicated.
which can lead to devastating birth injuries for babies, including death.
During labour, fetal heart rate monitoring can be used to monitor how the baby is coping with the stresses of labour. This can be completed by either CTG (cardiotocograph) or through intermittent auscultation with a doppler. It is crucial that the health provider follows the relevant policy and guidelines for fetal monitoring, particularly when there are risk factors and continuous monitoring is required. Alternatively, intermittent auscultation is the fetal welfare assessment method used for women who do not hold risk factors and should be conducted according to local policy.
Risk factors that increase likelihood of fetal compromise in labour and CTG is recommended. (NSW Health policy)
Antenatal (Pregnancy) Risk factors
- abnormal antenatal CTG
- abnormal Doppler (e.g. detection of fetal bradycardia)
- suspected or confirmed intrauterine growth restriction.
- oligohydramnios or polyhydramnios
- prolonged pregnancy ≥42 weeks
- multiple pregnancy
- breech presentation
- antepartum haemorrhage (bleeding)
- prolonged rupture of membranes (≥24 hours)
- known fetal abnormality
- Previous caesarean section
- pre-eclampsia
- poorly controlled or medicated diabetes
- fetal macrosomia
- other current or previous obstetric/ medical conditions which constitute a significant risk (e.g. cholestasis, substance abuse)
- reduced fetal movements
- morbid obesity (BMI ≥40)
Intrapartum (Labour) Risk Factors
- induction of labour with prostaglandin or oxytocin
- oxytocin augmentation
- regional anaesthesia (e.g., epidural, or spinal)
- abnormal vaginal bleeding in labour
- maternal fever greater than 38°C
- meconium or blood-stained liquor
- absent liquor following amniotomy
- prolonged first stage of labour
- prolonged second stage of labour
- pre-term labour less than 37 completed weeks
- tachysystole (more than five contractions in ten minutes)
- uterine hypertonus (contractions lasting more than two minutes in duration)

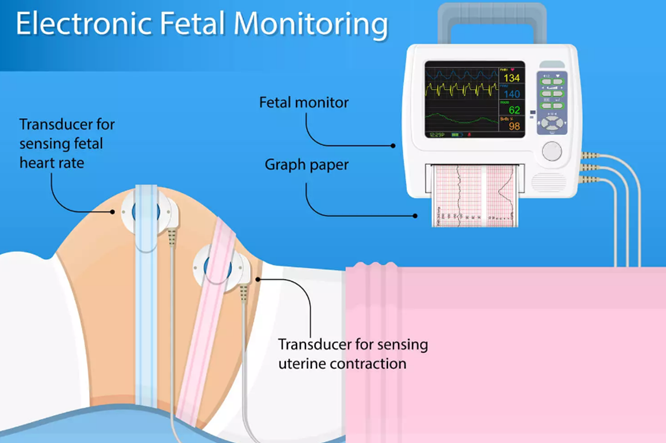
How does a CTG work?
There are two key elements to a CTG machine: a Doppler ultrasound which is used to monitor the baby’s heart rate, and a sensor which is used to monitor uterine contractions. These monitors transmit information to the machine which prints out a graph which can be interpreted by midwives and obstetricians.
In NSW, CTGs are considered according to the above algorithm, which is used by midwives to determine whether the fetal heart rate trace is normal, suspicious, pathological or urgent/ abnormal. These are a tool used to determine whether the clinical situation should be escalated to more senior midwives or Obstetricians for medical advice and intervention.
Abbreviations
- FHR: Fetal Heart Rate
- CTG: Cardiotocography
- Bpm: beats per minute
Heart Rate
The baseline rate is the average heart rate of the fetus.
- Normal baseline: 110- 160pm.
- Baseline Tachycardia: Greater than 160bpm.
- Baseline Bradycardia: Less than 110bpm.

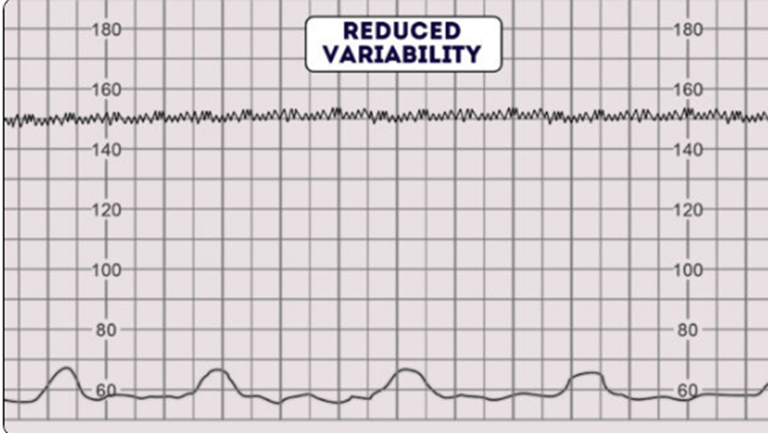
Variability
Refers to the variation of FHR from one beat to the next. It is a reassuring sign of an intact neurological system in the fetus.
Normal variability (Reassuring) is between 5 – 25bpm.
Reduced or Absent variability (non-reassuring) is less than 5bpm.

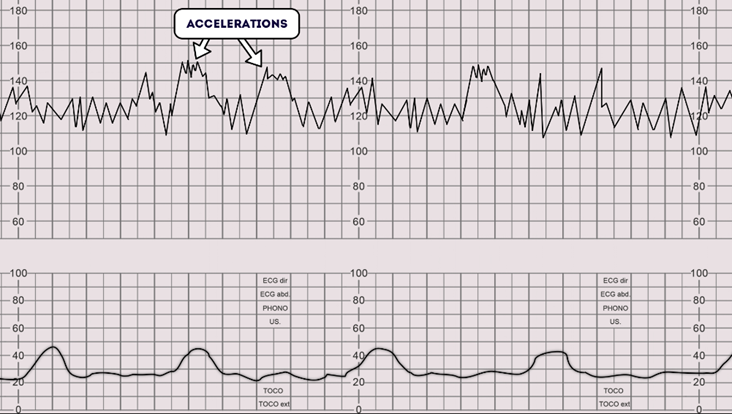
Accelerations and Reactivity
- An acceleration is an increase in FHR of 15bpm or more above the baseline, lasting more than 15 seconds.
- Reactivity: Present when there are two accelerations in any given 20-minute
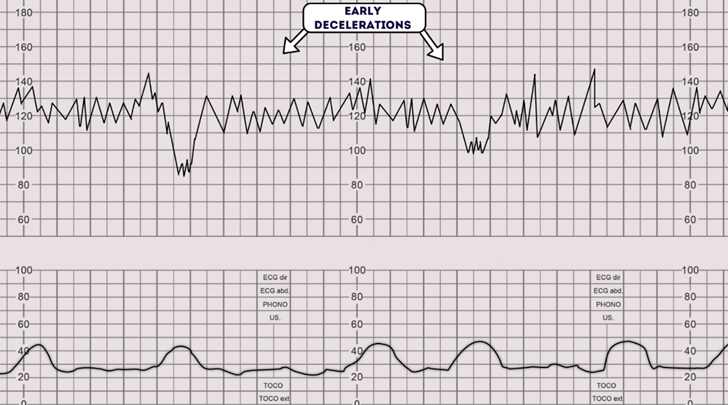
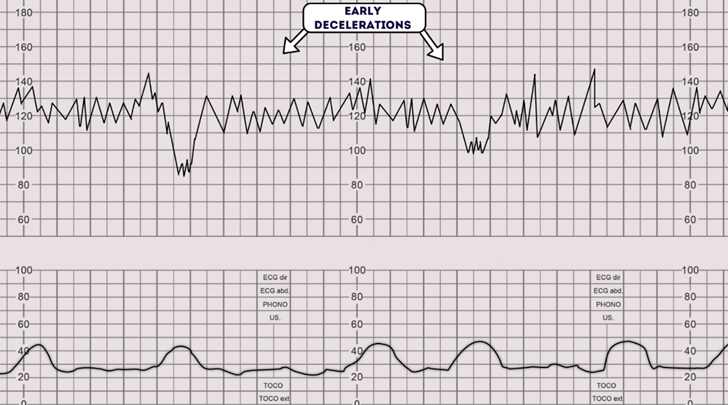
Decelerations
A sudden decrease in the baseline FHR of greater than 15 bpm for
longer than 15 seconds. There are a number of different types of decelerations.
Early decelerations are considered physiological, not pathological, as they are consistent with uterine contractions and resolve when the contraction ends.
Variable declarations are variable in duration and often do not have a relationship with contractions. They are often caused by umbilical cord compression. ‘Shoulders – brief accelerations on either side of the deceleration, are a reassuring sign that the fetus is coping.
Late decelerations occur after the contraction has begun and indicate there is reduced blood flow to the baby creating a greater risk of fetal hypoxia and acidosis. These are concerning and an obstetrician should consider if delivery is necessary for fetal welfare.
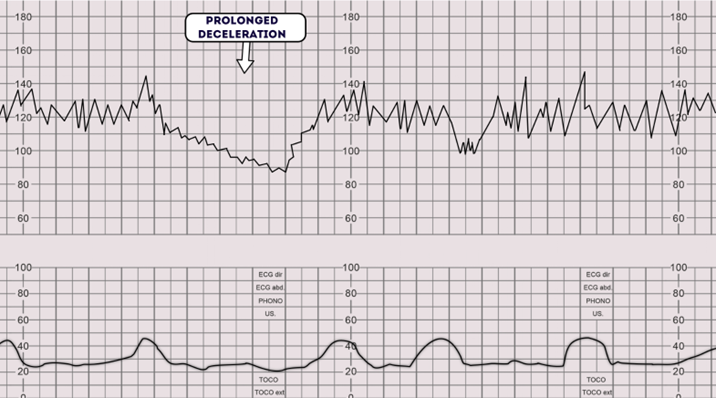
Refers to a deceleration that lasts more than 2 minutes, imminent delivery should be considered.
Uterine Activity
Normal uterine activity for women > 37 weeks gestation is 4 contractions or less in a 10-minute period.
Excessive uterine activity is:
- Greater than 5 contractions in ten minutes
- OR contractions lasting longer than 2 minutes in duration.
Without FHR abnormalities.
Uterine hyperstimulation (Tachysystole)
- Excessive uterine activity with FHR abnormalities.
Tachysystole is often associated with induction of labour processes, including synthetic prostaglandins and oxytocin infusion.
However, it can also occur in spontaneous labours where it can be even more concerning – occurring in association with placental abruption or intrauterine infection.
RANZCOG ‘Intrapartum Fetal Surveillance’

The CTG should not be used as a single tool to assess fetal wellbeing, but as an element to guide further management such as:
- Escalating to a senior obstetrician or consultant
- Assessing the clinical picture for obstetric emergencies including; cord prolapse or uterine abruption.
- Repositioning the mother or giving IV fluid bolus
- Fetal scalp blood sampling to test for fetal acidosis – a sign of fetal hypoxia.
- Bedside ultrasound to determine fetal positioning
- Expediting Delivery of the baby through emergency caesarean section, instrumental delivery, or vaginal birth.
Early detection of fetal distress is crucial for medical providers to resolve the critical situation in a timely and safe manner. Through prompt and skilled intervention, injury to the neonate can be avoided or minimised. However, failure to recognise signs of fetal distress can lead to permanent brain injury, disability or death.
Your medical provider should interpret, consider, and respond to any non-reassuring or abnormal features of the CTG with the required expertise, to meet the relevant standard of care. Failure to do so and as a result, your baby has suffered harm, would establish grounds for a medical negligence claim.
Photos: